Summary
From Holocaust Survival to Healing the Brain: The Legacy of Dr. Henry Brem
A 2024 CNS Honored Guest Lecture on Science, Humanity, and the Moral Imperative to Advance Medicine
Table of Contents
- Introduction
- Early Life and Family Roots
- Education and Early Research: The Birth of a Surgeon-Scientist
- The Folkman Influence: Seeds of Anti-Angiogenesis and Drug Delivery
- The Journey to Johns Hopkins
- Leadership, Growth, and Impact as Chair
- Mentorship, Values, and the Moral Contract with Patients
- Scientific Breakthroughs: Gliadel and Beyond
- Research vs. Surgery: Different Risks, Same Mission
- Legacy and Reflections
- Conclusion
- Key Takeaways
Introduction
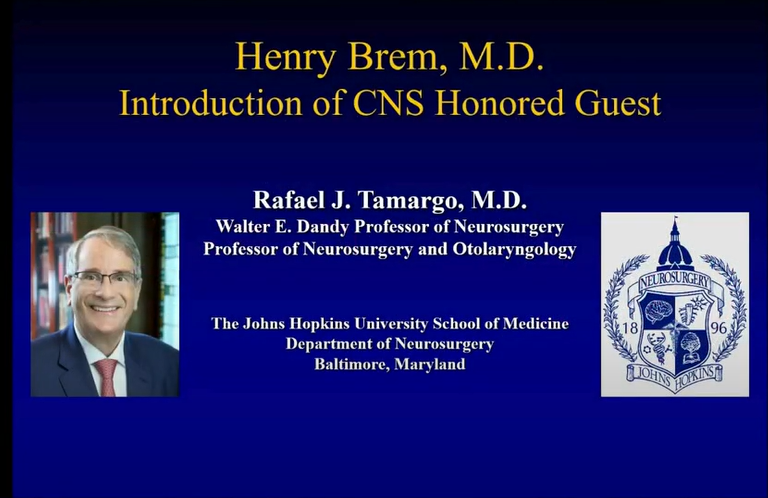
At the 2024 Congress of Neurological Surgeons (CNS), the community honored Dr. Henry Brem, Chair of Neurosurgery at Johns Hopkins, for his pioneering contributions to neuro-oncology, medical education, and translational science.
His life story — from the son of Holocaust survivors to a world-renowned surgeon-scientist — embodies resilience, moral purpose, and the pursuit of healing through innovation.
Early Life and Family Roots
Henry Brem was born in Paterson, New Jersey, in 1952, into a family that had already survived the unthinkable. His parents, Jacob and Adele Brem, arrived in the United States from a displaced persons camp in Germany after the Holocaust.
At just 20 years old, they spoke no English, had no formal education, and had lost their entire families — yet they rebuilt with extraordinary hope, faith, and joy.
From them, Henry inherited a moral compass rooted in:
- Tikkun Olam – the Jewish belief in repairing the world through good works.
- Compassion and gratitude – love for all people, despite the horrors they endured.
- Reverence for learning and teachers, values that would define his approach to medicine.
The Brem household embodied warmth, intellectual curiosity, and purpose — qualities that would later shape his leadership in neurosurgery.
Education and Early Research: The Birth of a Surgeon-Scientist
Henry excelled early. After attending the Yeshiva University High School for Boys in Manhattan, he went on to New York University, where he graduated cum laude in three years with a major in biology and a minor in English.
Even as an undergraduate, his fascination with cancer biology was clear. His thesis, “Mechanisms of Selected Carcinogen–DNA Interactions,” resulted in two early publications — a signal of the future scientific career that awaited him.
From there, he entered Harvard Medical School, beginning what would become a lifelong fusion of scientific discovery and surgical practice.
The Folkman Influence: Seeds of Anti-Angiogenesis and Drug Delivery
At Harvard, Brem joined the laboratory of the legendary Dr. Judah Folkman, a visionary who proposed that tumors depend on angiogenesis — the growth of new blood vessels — to survive.
Working alongside Dr. Robert Langer, Brem co-authored groundbreaking studies showing that:
- Cartilage contains an inhibitor of tumor angiogenesis, published in The Journal of Experimental Medicine (1976).
- These discoveries opened the door to anti-angiogenic therapy, one of modern oncology’s most transformative fields.
The trio — Folkman, Langer, and Brem — would go on to define how polymeric drug delivery systems could safely transport therapeutic molecules into the body, a concept that ultimately gave rise to the Gliadel wafer and later influenced technologies like mRNA vaccine delivery.
The Journey to Johns Hopkins
After completing residency at the Neurological Institute of New York, Dr. Brem joined Johns Hopkins University in 1984. Under then-Chair Dr. Don Long, he helped lead a small department of six faculty and 14 residents into what would become one of the world’s premier neurosurgical programs.
At Hopkins, he combined clinical precision with laboratory rigor, leading research on interstitial chemotherapy — the concept of placing chemotherapy drugs directly into the brain to overcome the blood–brain barrier.
Leadership, Growth, and Impact as Chair
Appointed Chair of Neurosurgery in 2000, Dr. Brem’s 24-year tenure transformed the department’s scale and influence.
Under his leadership:
- Faculty doubled to 24 full-time neurosurgeons.
- Resident positions expanded from 14 to 28.
- He raised over $350 million in funding.
- He created 15 endowed professorships and built a $50 million departmental endowment.
Perhaps most notably, he mentored 19 future academic chairs across the country — a legacy that ensures his values and vision will continue to shape neurosurgery for generations.
Mentorship, Values, and the Moral Contract with Patients
Dr. Brem’s moral philosophy in medicine is inseparable from his family’s history. His approach is grounded in empathy and service:
“The trust that patients and families place in us is sacred. That trust obligates us not just to heal, but to improve the inadequacies of medicine itself.”
He distinguishes between two forms of ignorance:
- Personal ignorance — not knowing what is already known (unacceptable in medicine).
- General ignorance — what science has yet to discover (the responsibility of research to solve).
To Dr. Brem, neurosurgeons bear a moral imperative to push beyond what is known — to make future care better than today’s.
Scientific Breakthroughs: Gliadel and Beyond
Dr. Brem’s most famous achievement came from decades of perseverance.
Through polymer research initiated in Folkman’s lab, his team developed the Gliadel wafer — a biodegradable implant that delivers chemotherapy directly into the brain after tumor resection.
Despite skepticism (“It will never work”), his group persisted:
- Overcame challenges in polymer synthesis and safety.
- Conducted one of the first placebo-controlled, multi-center surgical trials in neurosurgery.
- Secured FDA approval, the first for a brain tumor therapy in 25 years.
Even after approval, his advocacy continued — petitioning Medicare and Congress to ensure patient access.
Today, Gliadel remains a validated therapy worldwide, with ongoing studies showing survival benefits. Its creation represents not just scientific triumph, but the translation of moral commitment into tangible healing.
Research vs. Surgery: Different Risks, Same Mission
In one of his most striking reflections, Dr. Brem contrasted the worlds of surgery and research:
“Brain surgery follows rules — if you do everything right, you succeed. Research has no guarantees. You can spend your life pursuing a hypothesis that leads nowhere.”
While surgery offers immediate results, research provides enduring impact. Through his lab’s discoveries and the work of his trainees, Dr. Brem estimates that millions of patients have benefited indirectly from innovations born under his mentorship.
Legacy and Reflections
Dr. Brem cites Harvey Cushing’s 1929 ideal — that the best doctors are both practitioners and scientists — as his lifelong north star.
He reminds us that progress is never made in isolation:
“From flint drills to microscopes, from Pasteur to Langer — progress comes from countless fragments of applied knowledge crossing barriers.”
At Johns Hopkins today, that interdisciplinary spirit lives on through the collaboration of neurosurgeons, scientists, and engineers united by a single mission: to advance the boundaries of human healing.
Conclusion
From the ashes of the Holocaust to the heights of academic medicine, Dr. Henry Brem’s journey illustrates how faith, science, and compassion can coexist — and together, transform medicine.
His career stands as a living testament to Harvey Cushing’s vision: a neurosurgeon who heals with both the scalpel and the microscope, driven by empathy, intellect, and the unrelenting belief that every patient deserves better outcomes than the last.
Key Takeaways
- Heritage of Resilience: Born to Holocaust survivors, Dr. Brem’s moral foundation is rooted in compassion, learning, and duty to repair the world (Tikkun Olam).
- Scientist + Surgeon: His pioneering work in anti-angiogenesis and local drug delivery revolutionized brain tumor treatment.
- Moral Imperative: He sees patient trust as an ethical call to improve the science behind care, not just apply it.
- Leadership Legacy: As Hopkins Chair, he doubled his department’s scale, mentored 19 future chairs, and raised over $350M for research and education.
- Enduring Impact: Gliadel wafers, mentorship, and translational research continue to improve lives — proving that the true measure of a neurosurgeon lies not only in operations performed, but in lives made better.
Raw Transcript
[00:00] It's a tremendous pleasure to be here to introduce my close friend, mentor, and chairman, Henry Brehm. When Dr. Brehm asked me to introduce him, I was very touched and
[00:20] very honored to do so. So I will try to share with you the background of Henry Brehm so you understand why he is so deserving of this honor. I have no financial conflicts of interest regarding this presentation other than the fact that Henry is my close friend.
[00:40] friend and he's also my boss and if I don't say nice things, I won't have a job when I get back to Baltimore. So Henry and I have been friends and colleagues for 44 years. I met Henry and his wife, Rachel, the day before medical
[01:00] school started, Rachel was a classmate of mine and Henry was starting his residency. I was going into plastic surgery. I wanted to go into plastic surgery and I didn't realize that I was already getting mentored by Henry. He kept talking about neurosurgery.
[01:20] I am a neurosurgeon today because of Henry Brehm. This is Henry and me at the Columbia Medical School graduation. I joined the residency at Hopkins, followed Henry there. And this is in the middle of the residency. Henry is attending me as a resident. And this is
[01:40] What we do these days, hang around the pool with our grandchildren and dogs. Seriously, we have co-authored 31 papers together and I worked in Henry's lab when I started. This is Henry's chronology and I will go through it. He was born in Paterson, New Jersey.
[02:00] see in 1952 and for those of you doing the math right now, yeah, he's 45 years old and he looks great. His brother, Steven Brem, is also a neurosurgeon, as you probably know, and the Brem boys have always dressed up
[02:20] for the occasion. Here's Stephen and Henry, the two future neurosurgeons. Henry graduating from kindergarten. And as you know, Henry is always dressed for success. And here he was at the tender age of 7, I think, relaxing at home in a jacket and tie.
[02:40] high. Henry went to high school at the Yeshiva University High School for Boys in Manhattan, and it is my impression that this school had a tremendous impact on Henry. This is part of the mission statement of the
[03:00] the Yeshiva where they provide an outstanding education achieved through an unwavering commitment to serious Torah learning and rigorous study of modern science and the humanities. And Henry has more than fulfilled this mission. While he was there, he was chairman of the National Convention
[03:20] synagogue youth. So you see that at that early time he was already working on on being a leader. Henry then went to NYU and graduated in three years cum laude. At NYU he graduated in biology.
[03:40] whom Laude, he minored in English, which has helped him tremendously in writing the papers and teaching us how to write papers. He graduated early in three years, but took a lot of convincing, but Henry can sell ice to the Eskimo, so he did it.
[04:00] From this early time, he was laser focused on cancer. His senior thesis was mechanism of selected carcinogen DNA interactions. And he published two papers on carcinogens and their importance in biochemical pharma.
[04:20] ecology and cancer research. Henry then went on to Harvard University initially for one year in the graduate school in biological chemistry and then went on to a medical school. Here's a picture of Henry when he graduated in 1978.
[04:40] At Harvard, he had the tremendous insight and good fortune of joining the lab of Judah Folkman, who many of you know is a tremendous scientist who explored the role of androgenesis in so many ways.
[05:00] problems. Henry met at that time Robert Langer and Robert Langer is the distinguished professor of biomedical engineering at MIT and he was the force behind the polymeric devices working with these two men.
[05:20] Henry published landmark papers, three of which are this paper by Bremen Fochmann of inhibition of tumor androgenesis mediated by cartilage. They isolated the factor in cartilage that inhibits tumor neovascularization, which opened up a whole field of biologics in Canada.
[05:40] cancer. And then Henry worked on biocompatibility of polymeric systems and delivery of macromolecules. He then went on to do his internship at the Peter Benbrigham. Here's a picture of Henry in front of the brigham.
[06:00] with Rachel and also with his brother, Steve, who was doing a residency at the MGH. And then Henry trained at the Neurological Institute in New York under Dr. Stein and the illustrious group at the N.I. I have to say a word about
[06:20] Dr. Rachel Brem. Dr. Rachel Brem was a classmate of mine and he was a brilliant medical student and has had a remarkable career. She is Henry's partner not only as his wife but also his academic, scientific and management partner.
[06:40] She is, many say, the secret to Henry's success. Together they have raised a beautiful family. Most of them are here today. Rachel, among the many things that she's done, she runs a very impactful community.
[07:00] organization for breast cancer. And most recently published this book, No Longer Radical, explaining the new approach to breast cancer. Henry then went on to become a faculty member at Johns Hopkins.
[07:20] Here is Henry in the picture in 1984 with Dr. Don Long who was our chairman. When Henry joined the group, there were six full-time attendings and 14 residents. I'll come back to this in a second. I finish.
[07:40] finished my internship at Columbia and had the good fortune of going on through Hopkins to do my residency. But Henry and Dr. Long gave me the opportunity to work with Henry in the lab initially for one year and then two and then.
[08:00] and they kicked me out of the lab after three. Said you have to do a residency. But I had the privilege of working on the interstitial chemotherapy project. And these are some of the papers that we published with this. On interstitial chemotherapy, we showed in
[08:20] rats that giving chemotherapy directly to brain tumors in the brain was better than doing it systemically. With Michael Yang, a brilliant Hopkins student that went on to Harvard Medical School and is now an ophthalmologist in St. Louis.
[08:40] Cincinnati, we sorted out the released kinetics of the polymer. And then eventually, as most of you know, Henry carried out a placebo controlled trial showing that this made an impact. The impact was small, but it was significant and there's a lot more
[09:00] to be done and being done with this technology. His accomplishments are truly staggering. Henry has published 401 peer-reviewed publications and has an H index of 102. Most of you know that an H index of 60.
[09:20] is considered high for professors in the pure sciences. He's written, co-authored 61 chapters, co-edited four books, has 11 patents, 40 grants, 20 contracts, has received 60 major national and international awards, has made 590.
[09:40] national international presentations and in 1998 was elected to the Institute of Medicine of the National Academy of Sciences. In 2000, Henry became chairman of the department. As chairman of the department, he has grown, expanded what was a good department.
[10:00] and made it even more impactful. Here are pictures of Henry in the center as chairman in 2000 and then the picture this year, 2024. As chairman, he has made changes and has
[10:20] had an impact in a different realm. His leadership has always been wise and caring. In terms of statistics, he's doubled the size of the clinical full-time faculty. We have 24 full-time faculty. He's doubled the size of the resident staff.
[10:40] We have four residents a year and he has raised $350 million for projects in the department over 24 years and currently as he steps down as chairman is leaving us with an endowment of $50 million. He has created 15 new endowed chairs and
[11:00] Among the many aspects that can be used to measure the impact of an individual, he has trained people that are tremendous neurosurgeons and have succeeded in other areas like Dr. Schlosser, who just spoke and is having an impact beyond neurosurgery.
[11:20] But he has trained 19 academic chairmen in neurosurgery, six residents, six faculty members, two fellows, and five medical students. So in conclusion, it is a tremendous honor for me to present Dr. Henry Brehm.
[11:40] He has been my friend for many years, my mentor, my colleague, and it is a singular pleasure for me to see that he has been recognized as a major contributor in neurosurgery and is the honored guest of the CNS. Thank you very much.
[12:00] Thank you.
[12:20] CNS President Alex Kalesi and the entire CNS Executive Board for choosing me for this amazing opportunity and for giving me the chance to share with you a little bit of my own journey that shaped me into the neurosurgeon and neurosurgeon scientist that I am today. My disclosures are not
[12:40] directly relevant to today's talk. To understand my background, we need to go back to 1949. My parents arrived in the United States from a displaced persons camp in Germany after surviving the Holocaust. This photo captures a happy moment when my older brother Stephen
[13:00] who today is a professor of neurosurgery at Penn, and my parents, two remarkable individuals, came to the United States. At just 20 years old, they did not speak English, they had no high school education, and they had lost their entire families to the Nazi Holocaust. But they carried with them an
[13:20] incredible resilience and a joy for life and they rebuilt the family from nothing and our lives were filled with joy. Despite all they had endured, the unimaginable loss of their parents, siblings, and everyone close to them, they came to America with hope, ambition, and a strong connection.
[13:40] strong desire to build a better future. These are my parents, Jacob and Adelbram, with their four children, my older brother, Stephen, myself, my sister, Shari, who is a periodontist, my younger brother, Harold, who is a general surgeon at Rutgers. Our upbringing was great.
[14:00] grounded in the values my parents instilled in us. These values laid the foundation for how I approach medicine today. First, there was our heritage and what they brought over with them. There was a passion for learning, a respect for educators, a respect for how important our teachers were at every stage of our life.
[14:20] lives. Another principle that shaped me is the Jewish concept of tikkun olam, the idea that we are all responsible for making the world a better place. This belief has been central to everything that I have done. We were taught to strive to leave every situation better than we found it.
[14:40] There is also a very deep love of mankind and fellow human beings. This is despite the horrors of what my parents had survived and the worst of humanity that they had seen with concentration camps and death camps of murder. Yet we were brought up with joy, compassion, and love. In Hebrew, the expression
[15:00] is v'y'a haftelarecha kamocha, which means love your fellow man as yourself. And then we were brought up with a very deep sense of family, and this love of family also shaped me as a physician. And finally, on a profound appreciation for the value of life itself, there's a time
[15:20] communic expression, if you save one life, it's as if you've saved the entire world. And interestingly, that's on the plaque at the entrance to Johns Hopkins Hospital. This has been a driving force behind my career in medicine. In terms of understanding who I am, the most important person in my life is Rachel, my wife.
[15:40] life.
[16:00] in that time, either the Brigham or in us. Our life together is so much to find who I am both personally and professionally. We started off with most of our dates in Boston. We're in Judah Folkman's laboratory. Family has always been a big part of our life and because of that wonderful 46 year journey with
[16:20] with Rachel, we have three incredible daughters, amazing three son-in-laws, and 10 spectacular grandchildren that we are thrilled all live in the Baltimore, Washington area. As a physician, the deep love that I experience with my family gives me a deep empathy for my patients.
[16:40] and their families. I understand firsthand the profound emotional journey that families undergo when a loved one is ill and at this connection helps me care for them with greater compassion. When I chose a career in medicine, the work that resonated most with me was Impact, as in the theme of the double A and S tags.
[17:00] coming up. I wanted to maximize my ability to improve lives. I wanted to choose a path where I could have the greatest impact in neurosurgery, of course, was that path. The ability to change lives so dramatically through our work as neurosurgeons is extraordinary. Along the way, I've been inspired by incredible men
[17:20] centers, both in medicine and in science. The beauty of medicine lies in the seamless integration of science and humanity, and that has been endlessly fascinating to me. There were books that inspired me that I read as a college student at NYU that really were very important to me in building who I wanted to become.
[17:40] I was deeply moved by Christian Barnard, who lived in South Africa, and he carried out the first human heart transplant, taking advantage of incredible science and medicine and breaking barriers. The doctor's mayo, a father and two brothers who revolutionized American surgery. And then ironically, because I am the
[18:00] Harvey Cushing professor at Johns Hopkins that in college I was so inspired both by Cushing's biography and by his profound writings. Scientifically, I was very inspired by Pasteur what an incredible impact scientific discoveries could have on mankind. René Dubois wrote about the enthusiasm that God within.
[18:20] inspire science. And then my most important mentor is Judah Folkman, who I'll discuss further in a moment. In preparing this presentation, I revisited a lecture by Harvey Cushing from 1929. He highlighted the importance of blending science with clinical practice, suggesting that the
[18:40] ideal practitioners engage in both fields. And the quote is that, or among doctors, the scientists who may never see a patient and the practitioners whose work is based on the knowledge that comes from the many scientific laboratories and who indeed, if spurred by curiosity and given the proper training, may properly engage in scientific research
[19:00] research in medical practice at the same time, which is the ideal combination. So that was Harvey Cushing in 1929 describing how important it is to have both science and medicine in the same person. Interestingly, I couldn't resist sharing with you in that same lecture.
[19:20] He also talks about that in every generation, and again, please remember this is 1929 that he wrote this, every generation is prone to overvaluate its own accomplishments in the field that has lived through the most eventful era in history. So it's music to our ears to be told that the recent half-century
[19:40] which he's talking about in the 1920s, has seen the greatest progress of all. And then he goes on to say, but not everyone's entirely happy about it, and so on. So I think nothing's really changed on that front either. Mentorship is critically valuable. It's so much of how we pass on our knowledge and our approach.
[20:00] approaches. But it's not unidirectional. I think that the mentee and the mentor both invest major efforts and the outcome is phenomenal and transformative. My most influential mentor has been Dr. Judah Fokken, an incredible surgeon, scientist, teacher, and humanist who I'm incredibly proud of.
[20:20] indebted to. This is Judah Folkman and I at his house when I was a medical student. Years later when he was visiting professor once at Hopkins I tried to express to him how grateful I was to him for what he had given me and I said I wish I could somehow do something for you and he just
[20:40] And he was the kindest, gentlest person in the world. So I was surprised. He said, there's nothing you can do for me. Whatever you think that I've done for you, give it to your students, do the same. And that's always been my ideal. I don't think I've come close to doing for others what he did for me, but it has been my aspiration.
[21:00] aspiration. My brother Stephen has been a lifelong influence on me, inspiring me to pursue medicine as a career and to choose neurosurgery as a passion. His love of science and medicine was inspirational. Indeed, it was Stephen who introduced me to Judith Hochmann.
[21:20] major mentors for me that have inspired development as a surgeon scientist and so impacted on me are Arnold Pats who revolutionized ophthalmology he won the last reward for curing a major cause of blindness of retrolectrophyte or plasia through his research Don Long who revolutionized the understanding of brain tumor
[21:40] tumors in his PhD work and really nurtured an environment at Hopkins where a surgeon truly could devote himself to the laboratory as well as being a master surgeon in the operating room. And Mike Coven, who mentored me in oncology and pharmacology, to answer the questions that I was trying to address for brain tumors.
[22:00] Sal Snyder is a great neuroscientist and has been a major influence friend and mentor in so many ways and in helping build up some of the work that I'm going to briefly discuss. Lastly, my closest friend, Bob Langer. We both worked as students together in Judith Folkman's laboratory and both share Dr. Folkman as a mentor.
[22:20] Bob has done extraordinary work and changed the world from his research. This is a photograph from Dr. Fopin's lab in 1974. This is Bob Langer on the left of the screen and on the right. Dr. Fopin is in the middle, is myself and Dr. Fopin is in the middle. Bob Langer's work is not only the work that I'm going to do.
[22:40] going to briefly mention with brain tumors, but of course he's more than recently been one of the founders of Moderna. And with COVID vaccine, he's contributed to saving millions of lives worldwide, again showing the power of science. Reflecting on my journey, I think about the various phases that shaped my focus.
[23:00] medicine. At 18, I had the incredible opportunity to work in the Columbia Microbiology and Molecular Biology Laboratory with Herbert Rosencrantz, and I investigated the mutagenicity of alkylating agents while also gaining hands-on experience in the operating rooms in Columbia. In that summer, I published two papers on broad-
[23:20] hormone, is a carcinogenic agent and its mechanisms. That experience taught me a valuable lesson, that even with a very limited scientific background, if you narrow your research question down deeply enough, you can become an expert in that specific area and make meaningful contributions.
[23:40] This principle has guided me many of my scientific endeavors. When I had the fortune of working with Judith Folkman, I read his work and its hypothesis that angiogenesis was a critical control point in tumor growth. And while I was taking embryology in college, I came across the observation that cartilage starts off vascularizing.
[24:00] than the fetus and then the vascularity disappears. And having read so much about the theory of anti-angiogenesis and talking to Dr. Fokker about it, I said why don't we see if at the point that it loses its vascularity, that observation in nature maybe has an active inhibitor for angiogenesis. Make a long story short, we spend a year with the patients.
[24:20] year working, Dr. Folkman's laboratory and this was the key finding that cartilage was in fact had an inhibitor for angiogenesis. This was published in the Journal of Experimental Medicine. It was the first description of an inhibitor of angiogenesis. And just parenthetically, this paper was cited by the American College of Medicine.
[24:40] surgeons is one of the hundred landmarks of surgery in the past century. Looking back, anti-agendesis has had a profound impact on ocular disease and dermatology and of course on cancer and I'm proud that I had a role in initiating this process and even more importantly in most what I want to emphasize in the past.
[25:00] is that surgeons were responsible for initiating this scientific and clinical changes. Bob Langar joined Dr. Fokpen's lab as a postdoc fellow. He purified that material from cartilage, and that was published in Science. And then stemming out of that work, Bob Langar and Judith Fokpen wrote the first paper in Nature on polymers for the system.
[25:20] sustained release of proteins which really effectively created the field of drug delivery. Later together with Dave Tapper, who later became the chairman of pediatric surgery in Seattle, we explored how to make these polymers safe for human applications. I was very excited by science, but I was really thrilled to be in medical school.
[25:40] And as I looked back at medical school, in addition to the incredible excitement at working with Judah Folkman and others, it was really about learning and mastering medicine and a tremendous amount of effort and time to mastering the scientific clinical sciences, enabling me to provide the best care for my future patients. Judah Folkman frequently
[26:00] spoke about the distinction between personal ignorance and general ignorance. Personal ignorance is failing to know something that is known information. You're the one who doesn't know it, but everybody else does. And that's unacceptable because you could potentially harm a patient when it was preventable.
[26:20] intolerable. In contrast, general ignorance encompasses the scientific questions that we still need to answer through research, like how do we cure glioblastomas? As a neurosurgeon, I have always felt a profound trust for my patients. They allow me to care for them and to perform
[26:40] surgeries, placing their faith in essentially a stranger to help them through some of the most vulnerable moments and yet they trust me enough to allow me to do my best given our best available knowledge to help them. One of the things that I've learned over time, so we used to say that you treat people the way that you want.
[27:00] to be treated. What I've learned over time is that's not enough. It's not high enough standard. The standard really is to understand how they, the patient, want to be treated and to make sure that you're meeting that expectation. Well, medical school was really devoted to focusing on specialty, learning and picking a specialty that I wanted to be treated.
[27:20] devote myself to and that became, of course, neurosurgery. My residency at Columbia was really six or seven years of just incredible devotion to learning neurosurgical anatomy, pathophysiology, and of course the incredibly demanding techniques that are required and which consume my entire focus during that time period. When I first started out as a nurse, I was a nurse. I was a nurse.
[27:40] first came to Hopkins, I knew that I had this incredible scientific background. I had worked with great people and I was fascinated by science. But I knew that it was very rewarding, but I understood that the impact it could possibly have. But I spent seven years learning neurosurgical technique and I had to take care of neurosurgical and how to
[28:00] take care of neurosurgical patients, and I knew that it was exceptionally rewarding and demanding. I felt a little nervous about taking care of patients independently when I first started, maybe not just when I first started. Could I take care of patients and do brain surgery and spine surgery? Would people trust me to take care of their patients? Could I be a good doctor?
[28:20] care, not as a resident, not under someone else's supervision, but on my own. So when I started as an attending at Hopkins, I was very focused on building a practice in building special relationships with my patients. I would wake up early before I would do an operation. I'd restudy the anatomy, the technique. I was very relieved into life.
[28:40] And I did that very quickly. I built up a trustworthy reputation and I built up a practice that physicians and other patients would come to me, particularly for brain tumor surgery, and that had a very large practice. And that people trusted me and that I fulfilled that trust that I did the best that was available in medicine and in neurosurgery at that time.
[29:00] time. But after a little while, after the relief that yes, I could do these things that I was taught to do and that could achieve the best results of our specialty, and that was very satisfying. But I began to realize it really was not enough. And I realized that there was a huge emptiness from it.
[29:20] because I realized that patients were coming from great distances, for example with malignant brain tumors, and I became very close with those patients and they trusted me. And I worked with them and I helped them and their families and we formed these incredible bonds, and then they died. And I realized that with all the work that I was doing and all the
[29:40] the trust that they had put in me, the outcome was still totally unacceptable, that we just didn't know how to do better. And I was close with these patients and I asked them if they felt like I had let them down. And the answer that I started to get was no. We understood that there was no cure for this and we know that
[30:00] You're working on making it better. You're a Hopkins scientist as well as a neurosurgeon, and that's okay. We want to be part of that process of making the outcomes better. And I realized that I had a contract with these patients and a responsibility to those patients, not only to do my best and the field's current best.
[30:20] But I had to find ways to do better. And that's what was expected of me. And that's what I had the opportunity and the training to do. So after an initial period of practice, there was an understanding that it just wasn't enough. And I felt like, yes, I really could operate expertly. I could do what I was trained to do and what the future.
[30:40] real laws at the time, but it really wasn't enough to do that. And I also realized that we just needed to do more is the bottom line. If the goal is cure, then we basically fail. And that's true in so much of medicine, extremely so in the glioblastomas that we take care.
[31:00] care of, but really in much of medicine that's true. However, if the objective is to improve the outcomes, then we do succeed. We succeed both by our clinical expertise and compassionate, meticulous care of the patient and our families and our friends. And speaking with my patients and even the ones who die in a year
[31:20] and do not and do have this terrible outcome, they're grateful that I and the whole team were there with them in the process and that we were always there for them, we helped them, and we're not abandoned. They understood that we don't create the diseases, but we can really help people deal with them as they go through the process.
[31:40] But the real moral obligation, the real change that I felt had to happen, was to really change these outcomes. I felt that had to happen. We had to create even incremental advances in measurable outcomes. And then one more sort of side point in thinking about these different things about what makes
[32:00] us who we are. I think that to some extent, as much as I care so much about people and I do deeply care and I care about my patients deeply, we also do create a psychological shield to create some distance from the pain and the suffering because it's overwhelming how much suffering that some of our patients go through.
[32:20] sort of think they are the patients and they're over here and we are the physicians and we take care of them and I think that's what gets us through. That's how we can go home and be with our family or go to a lab and do research, how we can walk away from the pain and suffering that we also are involved with when we're with our patients.
[32:40] really good at compartmentalizing. But despite that sort of psychological shield that we put up, some patients penetrate that protective shield, and they make us feel they're suffering very deeply. And then we struggle to stay clear-minded and objective. If that shield is broken, it's hard to do some of the hard things that we have to do.
[33:00] But feeling that suffering is a very strong motivator, and it does constantly remind us of how serious the problems that patients are facing when they come to us and when they get our help. So I've come to believe, and I've used this term before, that there's a moral imperative to give back.
[33:20] or the trust that patients and their families put in us. That trust obligates us to do research and to improve the inadequacies of medicine and surgery. When one chooses which way to go in your career, I've also come to realize that interestingly, that in many ways, research for a career is, in some ways, much higher risk than brains.
[33:40] surgery. And I say that and I know people laugh when I say that, but the reality is that brain surgery is a body of knowledge that you learn, you study, you work at, you learn techniques and you follow the rules, you do what can be done, and there's very little personal risk, career-wise, to the person if you're within the guidelines of what's acceptable in neurosurgery.
[34:00] On the other hand, in a research career, you could spend your whole life working on a scientific hypothesis. You could work day and night. It could turn out to be nothing. It could turn out to be an artifact. It could turn out to be meaningless. So in fact, the risk, career-wise, is in a sense much greater in research. If your goal is to be impactful, you could really spend
[34:20] lifetime in a laboratory and not be impactful. By contrast, the consequences of neurosurgery, what I do clinically, are immediate and very great to those patients. However, the impact I think is much greater in research, the potential impact, and I would even say that as I look back at my own career. Although I have held
[34:40] help thousands of patients by operating on them and taking care of them, and the positive satisfaction of neurosurgery is enormous, but I've impacted even more patients in an indirect way through the research that we as a group have done. Mentoring our trainees to follow this combined pathway has even
[35:00] further increase the impact through their subsequent work, which reinforces Harvey Cushing's ideal of combination of the practitioner and the researcher. Many more patients have benefited from our discoveries and our findings than I've ever seen as an individual neurosurgeon. So it's interesting that the two aspects of our
[35:20] careers have very different risks and benefits to them for the people who practice them. I thought I'd take a few minutes and just go through a little bit of the ride with brain tumors that I've taken. I'll do this very quickly. I don't want to fall into giving a scientific talk, although I'd love to, but I will share a little bit of the ride with brain tumors and I'll try to
[35:40] to do this very quickly. One example of the work that we've done is a delivery of therapeutics. When we started the problem with clinical ineffectiveness of every new cancer therapy which doesn't even get to the tumor and does it hit the proper targets. We have hypotheses
[36:00] exercise that maybe they just weren't getting to where they needed to go. And we used the polymers that had been developed with Langar Group at MIT for drug delivery, which had never been used in people before. And I'll just be very brief. This is Ian Sook's beautiful drawing just showing that we needed to get across the blood-brain barrier. We put together a multidisciplinary group at
[36:20] Hopkins, this is from our first NIH grant. It's a million dollars a year for over 20 years, and it worked with pharmaceutical company Nova, which was Sal Snyder's initial company, working with pharmacology by medical engineers and so on. Raphael Tomargo, who so graciously introduced me, who is now the Walter Dandy professor.
[36:40] of neurosurgery and head of our vascular service. But as a fellow, he worked with us and helped develop these models, which are shown here. We'd implanted brain tumors in these rats. We then showed that and infused drugs in various different ways. We looked at Kaplan-Meierkirch.
[37:00] showed that with a polymer we could get even better survival than the same drug given systemically. And this is a gliadale wafer. This is a patient where we've taken out the brain tumor. We lined the resection cavity with carmustine wafers and they released chemotherapy over a period of weeks.
[37:20] But this approach was effective and had a statistically significant improvement in survival. So it's very interesting when you look at how things develop that, and I just take a moment to share this with you, that as Bob Langer and I and colleagues at Hopkins were developing this approach and presenting it at meetings,
[37:40] things, we found that it would be very well received. People respected the work and they said it's really cool work, really good science. I have the next slide. But they would add, but you know it will never work. And what was interesting was that over the years it was always a different reason that we were told after we presented.
[38:00] presented the work that why it was impossible. So we put this slide together to just show sort of in that journey that there were constant critiques. First they said the polymers couldn't be synthesized, they'd react with drugs, they'd be fragile, they'd be toxic, they wouldn't diffuse far enough. So we answered and we got more data. We didn't get angry. We didn't
[38:20] drop it, we just said, okay, we'll show you. We'll test it, we'll go back to the laboratory, we'll develop it. And we did all these things and we published them in, you know, top-notch journals and we just systematically answered the questions. People then said, well, you know, models, you know, animals don't reflect clinical reality, anybody can cure cancer in there.
[38:40] mice, but that's not what's going on with people. So we did the clinical studies. And we used the same rigor in the laboratory that we did in the clinical studies. And it was very challenging to do so. We did a randomized prospective placebo-controlled study in 27 medical centers. And in doing so, we showed the
[39:00] FDA that we really had something that was beneficial for patients. The FDA approval was thought to be impossible. They hadn't approved anything for brain tumors in over 25 years. But we showed that we could do that. And then I was shocked that once it was approved by the FDA, I really thought my job as a neurosurgeon was done.
[39:20] Medicare wouldn't pay for it, so we had to really go public. We had to petition Congress, we had to get political support, we had to get Medicare to make it available to patients, and then there were other issues that kept coming up. We received approval for both recurrence and initial therapy from the FDA in 2003, and we more than doubled the median rate.
[39:40] median survival. And that data is, you know, for many years ago. But even more recently, in 2023, there are studies being done with gliadis and comparing it with current therapy. Here's an example in France with 1,600 patients, 42 institutions, and showing statistically significant improvement in survival. And so
[40:00] their conclusions were it should be a standard therapy for malignant glioma. We have, of course, there's an enormous need for better approaches and more effective approaches. We've studied many different approaches in targets and delivery devices over the last 40 years, and I'm optimistic that many of them will
[40:20] significantly impact patient care and improve patient care. I'd like to share several examples of this promising new approaches with you in my afternoon talk at the luncheon. Many examples of where we've gone back and forth to the laboratory and we're going to improve the care for our patients based on testing.
[40:40] ideas and developing new ideas in the laboratory. So in conclusion, research progress is not the same as in surgery. In surgery, when I take out a brain tumor, the patient goes home, it's wonderful. The patient benefits immediately, we see the results of our work immediately, and they benefit from the action.
[41:00] Progress in the laboratory is incremental. That progress only happens if you stay focused and persist with relentless effort. And I'll conclude with going back to Harvey Cushing in his 1922 where he talks about the neurological advances, the dependence on cognitive disease and cognitive disease.
[41:20] Not only on the great works of this specialty, like specialists like Jackson, Horsley, Sherrington, and of course himself, but on a multitude of laborers and other arts and sciences, the connection of which was not at first obvious. Faraday, Bessamra, Edison, Crookes, Rendtke, and Lister, Pasteur, Simpson, other workers with the might
[41:40] microscope chemistry, and so on in an endless chain. The progress from the days when a piece of flint was drilled into the skull to let out the evil spirits to the present time, 1922, when a brain tumor could be detected and removed, was merely the result of adaptation of innumerable fragments of applied knowledge.
[42:00] knowledge of crossing barriers and working across silos. Harvey Cushing and Walter Dandy's legacy lives on at Hopkins and is vibrant in our extraordinary specialty of neurosurgery. We have an incredible group of people at Hopkins and it's not a one
[42:20] man show like it was in Harvey Cushing and Walter Dandy's time. It's an incredible group of devoted people, all with the same mission, that of helping people to the maximum way through clinical work and through research. The greatest satisfaction has been for me in mentoring the next generation.
[42:40] to both master our exciting field as neurosurgeons and to advance it significantly.
[43:00] brilliant students and residents, faculty, and a tremendous trust from our patients that allow me to both take care of them in the best way that we know how to, which is good, but not good enough, but also they give me the stimulation to move the needle forward. Thank you very much.
[43:20] APPLAUSE